Pneumonia Ultrasound Diagnostic Strategy
In June I will be travelling to the Emerald Isle to attend and learn at the SMACC Conference in Dublin. One of my jobs whilst I am there is to help out on the SMACC Mini workshop – I will be talking about using lung US to diagnose paediatric pneumonia. Clearly, I am a self-confessed sonophile. I think that we can get a lot of information in quick time by using the bedside scanner to interrogate the lungs. BUT, there is always a BUT… what we do with this information is most important. Lung ultrasound is really very simple, technically easy and there are not many subtle anatomical findings to keep you guessing. However, when we interpret our scans we need to know a few things:
- What is the clinical question? Are we “Diagnosing” or “excluding pneumonia”, “Septic screening?” or “differentiating pneumonia from bronchiolitis?”
- Do the findings represent “hard” or “soft” signs of pneumonia – could the signs be false positives?
- What is the plan – are we going to act on our findings? Hit then with antibiotics? OR get more tests?
Dr Rory Spiegel posted a great critique of the recent evidence around lung US for pneumonia at EMNerd this week. “A Case of Shadows II” His post has prompted me to respond by explaining how I think we should use this tool in the light of our current evidence.
If you read the abstracts you will come away with a somewhat “black n white” view of the world. However, there are a few shades of grey. You will read impressive numbers – a positive likelihood ratio of 15, a negative LR of 0.06… this is a great test! It discriminates in both directions. BUT… here’s the next BUT… you need to know what these investigators were calling “pneumonia” and what was not. If you have done any lung scanning you will know that there exists a spectrum of findings -ranging from hard to soft. So where on this spectrum can we “call it”?
- Hepatisation with dynamic air bronchograms
- Hepatisation with static air bronchograms
- Large subpleural consolidations
- Sub centimetre sub pleural consolidations
- Unilateral B-lines
- Unilateral effusion
Classic hepatized lung with “shred sign” of adjacent B-lines
Basal pleural effusion
The diagnostic characteristics of these signs are not all equivalent – as you go down the spectrum they become less specific [and more sensitive]. This does not make them useless – just less potent as far as diagnosis goes.
There is also a real risk of over-diagnosis if we start overcalling pneumonia based on the softer signs. So how do we integrate this “new test” into our practice? I reckon we need Bayes. We need to be smart about how we use the information that US provides.
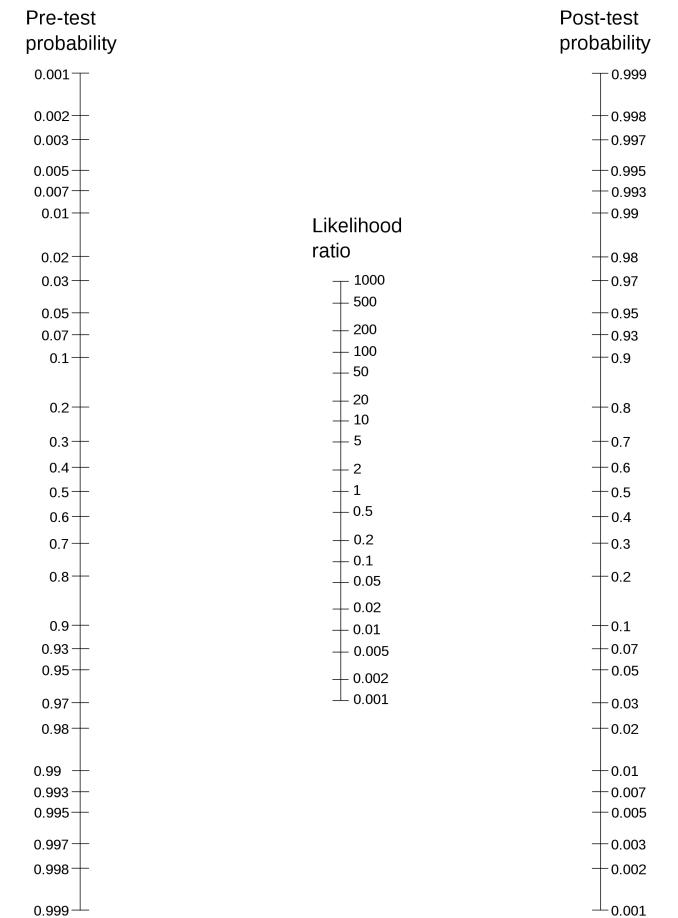
Lets start with a case. Here is the pretest- probability guesstimation:- we are not great at picking pneumonia clinically – however if we have a child with fever, cough, tachypnoea and unilateral auscultation changes then I would guess that we are at about 50% at least. So lets whip out the nomogram! If we start at 50% and have a hard sign (e.g. dynamic air bronchograms) – +LR around 15 then we are up to about a 94% post-test probability – this is a slam dunk, I think we would all start treating this kid. If we were to see only a softer sign such as focal B-lines and a tiny unilateral effusion then our +LR is weaker ( wild guess would be about 5??) That still gets us to a post-test probability of 83% – and I would start antibiotics at that level. [Editorial note: these numbers are completely fictional. Based on my own experience and reading. We need to have studies that exam these signs].
If you decided that the chest wasn’t convincing on auscultation – then your pretest risk might be lower – let us call it 20%. In that case a soft +LR of 5 would only get you to 55% post test… maybe not good enough to call it over the “treatment threshold”. We need more data.
So lets consider another scenario. 2 year old girl with fever, poor perfusion and tachycardia. No localising signs on examination. We are definitely going to start empirical antibiotics based on her risk of sepsis. But we want to run a “septic screen” to find the source. In this case our pretest probability is lower. Maybe 10 or 15% chance of pneumonia. So a CXR probably has a sensitivity of 70%, is that good enough? Our lung US can have a whole range of sensitivities. If we draw the line at “completely normal” – i.e.. none of the hard, soft or indeterminate signs listed above then the data suggests a sensitivity of high 90s. So our strong -LR in this setting allows us to get our post-test probability down, well below 1%. We need to look elsewhere for the source, maybe she needs an LP?
Now – a tougher case. A 12 month old boy who has been admitted with bronchiolitis fro 48 hours. He was initially improving with supportive care, but today has developed increased fever, tachypnoea and oxygen requirements. He isn’t following the usual branch curve. Has he developed a superinfection / pneumonia? Lets scan his lungs…. We expect to see bilateral, small (sub centimetre ) sub-pleural consolidations. Maybe symmetrical, small basal effusions. So here we need to be choosy. I would ignore any of the softer signs listed above. There is a low signal:noise ratio here. For our scan to be useful we would need to see a hard (very specific) sign of pneumonia – such as a larger area of hepatisation with air bronchograms to allow us to make a call. In terms of post-test probability, out treatment threshold need to be considered. Given the clinical situation is the best option to start antibiotics.
Lung ultrasound is a test. Like all tests it has imperfections. It is not a binary phenomenon – there are a range of “cut off points” that you can use to enhance its ability to rule in or exclude pneumonia. Unlike a numerical test like troponin or D-dimer it is not as simple as shifting the magical “normal range”. We need to understand the relative potency of all of the possible findings and use these to our advantage depending on our goal.
So go on! Use lung US in your practice. Use it wisely.
- Think about the context of your patient, estimate the pretest probability.
- Decide if you want a sensitive or specific test – what are you trying to do? Rule in or out?
- Scan and interpret you findings – is it negative? Or maybe soft? Hopefully you find some hard signs.
- Understand how to apply these findings to the patient
- Premeditate your treatment threshold – at what level will you be starting treatment?
The best thing about lung US is that you can play around with it and only waste a few dollops of gel and your own time. There is no real inherent risk in the test itself – no radiation or the need to bother the nice radiographers!
I hope this all makes sense. Let me know if not!
Cheers
Casey



I think you’re right to talk about both pre-test probability AND the “gold standard” of CXR or clinical exam as comparisons. We can and should have the same conversation with pre-test probability and CXR, and we all know that 1) we have sometimes been surprised by what we see on X-Ray and 2) most of the time it involves squinting and guessing if you “call” peribronchial thickening and streakiness vs consolidation.
There will clearly never be a study comparing lung u/s to chest ct in kids (at least not large and randomized), and the reality is that most pneumonias would probably clear clinically regardless of antibiotic use, so the high quality studies are going to be difficult.
Thanks for posting and good luck teaching in Dublin!
Hey Casey,
Great summary. I’ve struggled with this myself, and tend to do the exact same thing (dynamic air bronchograms: treat; Softer signs: clinically correlate).
What we need is a larger (hundreds/thousands) of patients to see which signs are more specific for PNA that needs treatment. For now, its going to have to be up to the individual clinician (like many other tests)