SAFE Sedation Guide
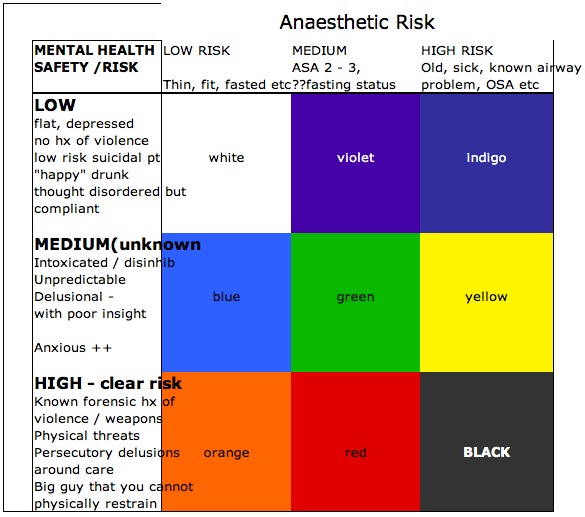
So here is how I reckon you should manage / sedate each of the groups (colours) in the SAFE Sedation matrix. Some of tis is not new – there are a few strategies that are not routine practice – let me know what you think:
WHITE: low-risk in both ways – if you are admitting these patients then you may need a sleeper, or mild anxiolysis only – easy, do your usual thing.
VIOLET: in this group I would advocate restraint, monotherapy, longer-acting agents and good nursing are all that is required.
INDIGO: Step away from the drug cabinet! You have little to gain from sedating a high-risk medical patient who is not too agitated. Good nurse care, orientation, reassurance and minimal stimulation are best – enlist family where possible
BLUE: This group need some sedation. The strategy I like with the healthy / thin patient is a decent dose of sedation – then see what happens – either you are good or you add a bit more – I like a combo of antipsychotic and benzo (eg, Olanzapine + Clonazepam). The mistake I see often is trying a little dose of x, then swapping to y, then z – suddenly the patient has subtherapeutic doses of 3 agents on board and it is hard to decide what to do next wen they don’t work!
GREEN: This group is the same management as BLUE – except you might want to do it in an environment where you can do airway stuff if needed whilst you are titrating. If you have time then titrate the sedation (something longer-acting), try and achieve fasting, maybe some metoclopramide and PPI for the reflux?
YELLOW: This group is tiger territory – their safety risk is either unknown or volatile – but you know they are likely to be an airway problem. I think here you should use non-pharmacological means first, try a small dose of shorter agent (eg midaz) and then a tincture of time. Two things might happen – either they settle and become “INDIGO” or they don’t – then you are looking at BLACK – see below.
ORANGE: This is the controversial bit. Thin, healthy, easy airway BUT very dangerous / violent punter – traditionally we have used big doses of all sorts to get them under control…. and then intubated them as there is no way the RFDS will fly this guy unless he in in a coma (quite sensibly). So my PROPOFOL as first line comes in here – why put the patient at risk with a day or two of heavy sedation / airway unprotected, urinary retention, staff being punched wen you can just jump in with what you are going to have to do eventually anyway? Sure talk to the RFDS team, arrange a transport, keep the Police in the department / handcuffs on etc until you are ready then – RSI, Propofol / fentanyl drip. Off to ICU for wake up then into a secure facility – minimise the risk to all parties.
RED: Same as ORANGE – but you might want to optimise your situation – await fasting if you can, have the best airway team you can get there. Keep the patient in the critical area / Resus bay with Police etc nearby. You might try a bit of sedation, but only if you are prepared to “go all the way” if the need arises
BLACK : “Damned if you do, damned if you don’t”. I am gonna post a case that falls into this category to illustrate the disasters that can occur in this area. Needless to say it ended very badly. My suggestion is to use the minimum drugs you can and have both a good airway setup / cric kit etc all there. DO not let the Police leave – handcuffs might be nasty but they are better than being dead. This is tough – there is no good answer – I will put up my case for comment soon. All I will say is I would rather be pulled up by the Mental Health Advocate legal team for being cruel with physical restraint of a live patient; than face the coroner about the sedation that resulted in the death of my patient….
1/ Thanks Casey I agree this area is a minefield and debate is to be commended. I like the matrix model to assess risk.
2/ I would recommend avoiding metoclopramide in these patients.
My personal bias is maxolon is a cheap drug which has lots of side effects and risks and the benefits may be more theoretical than real.
Maxolon has the potential for dangerous interactions with antipsychotics.
Most of these patients will get some form of dopamine antagonist (typical or atypical antipsychotic).
There is a risk of EPSE with all dopamine antagonists, especially with high doses or combinations of multiple agents.
Also akithisia and other muscular side effects can be very unpleasant for the patient.
Apparently there are reports of acute dyskinesias so severe as to impair breathing. Psychiatrists sometimes prescibe prophylactic benztropine (in patients on high dose dopamine blockers) because they are worried about this.
I would suggest if you want to use a drug that will theoretically reduce the risk of aspiration in an acutely agitated patient stick with vitamin H.haloperidol (ed) (or even better droperidol if they have normal QT).
3/I agree we should probably use more physical restraint.
However, when I worked in Derby they had this device which was a cross between a straight jacket and doona – you could strap them in then they couldn’t move anything except head and neck. It attaches to the be rails.
They have a protocol and it is legal.
The rule is apparently you are allowed to use physical restraint after you have made a risk/benefit assessment and notified the office of the chief psychiatrist (fax will suffice)
It was truly, truly awful to watch an agitated confused person being restrained in this way.
Reminiscent of “one flew over the cuckoos nest”.
I then thought poor bastard shall I give sedation to ease their distress, but that is a really slippery slope when patient has threats to airway & breathing both physically and chemically.
4/ No easy answers.
Thanks Yehuda. All good suggestions. I did not go much into physical restraints, I will do so when I post my next case on the “Code Black” Psych situation.
I also dislike the old dopaminergic drugs, they are not very clean -I pretty much reserve them for the patient who is already on them (supposed to be on them).
Benztropine – well my evidence is level 7 (my sister told me – she is a MH nurse). Those at risk include: previous reaction, young, healthy people, men > women. In her place they do not routinely give it unless the patient has a history of EPSE. If somebody has a dystonic reaction / EPSE then they should be treated with IM / IV benztropine as it can progress quickly. I think there is not much downside to oral prophylaxis in the risk groups but it will wear off before the haloperidol is stopped. I did find one article that showed using promethazine with haloperidol reduced the risk to similar levels as seen in atypical agents – so maybe a bit of Phenergan is the way to go?
Hi Minh,
Thanks. The Sedation matrix I published on the blog is the result of a lot of personal brainstorming for a lecture I gave in 2010 to the FACEM conference here in Broome.
There is no evidence – just logistical murmuring and a lot of trial and error. I have not seen the Qld matrix, please send me a link if you have one.
The goal of the heavier sedation used for high level agitation is a relatively flat sedation profile, avoiding the peaks and troughs where the “vomit is aspirated and the punches are thrown”.
Gotta say I am using less Midaz infusions – as I notice they tend to get turned off by well meaning nurses and then you have an awake / disoriented patient, or they tend to be overdone – resulting in aspiration, or the drip fails and goes unoticed until it is too late! They are good in theory, but in practice can go seriously awry!
I will put up a case of a “Code Black” patient I was involved with on several occasions – will illustrate many points and pitfalls.
Love ketamine – but not used it in Psych – please send me your paper, would love to read and critique.
Thanks for your pearls, will take up the surgical airway debate with you soon!
Casey